RG specialist recognition
The two stages of assessments have been conducted over several years by the Australian Medical Council (AMC). The Rural Generalist Recognition Taskforce chaired by the National Rural Health Commissioner Professor Jenny May has continued to oversee efforts toward achieving recognition.
Rural Generalist Recognition - Progress Update | Feb 2025
Rural Generalist Recognition - Progress Update | Dec 2024
Rural Generalist Recognition - Progress Update | Oct 2024
Rural Generalist Recognition - Progress Update | Apr 2024
Rural Generalist Recognition - Progress Update | Oct 2023
Rural Generalist Recognition - Progress Update | Jul 2023
Rural Generalist Recognition - Progress Update | Dec 2022
Rural Generalist Recognition - Progress Update | Sep 2022
Rural Generalist Recognition - Progress Update | Jun 2022
Rural Generalist Recognition - Progress Update | Apr 2022
-
2023AMC assessment panel formed
-
2022Stage 2 joint application for RG Specialist Recognition submitted to MBA
-
2021Second round of advice submitted to the MBA.
-
2021National RG Strategic Council of which ACRRM is a member formed to progress the broader National Rural Generalist Pathway agenda.
-
2020RG Recognition Taskforce conducts further national consultation.
-
2020MBA requests further actions and information.
-
2019Joint-application for RG Specialist Recognition submitted to MBA.
-
2019RG Recognition Taskforce formed (ACRRM, RACGP, National Rural Health Commissioner) to progress joint-application
-
2019NRGP Advice tabled with Parliament
-
2018National RG Taskforce (NRGT) Advice on implementing a National Rural Generalist Pathway developed following national consultation. Recommendations include seeking RG specialist recognition
MBA application Stage 2 | Dec 2022
MBA Application Stage 1 - Additional Advice | Jul 2021
MBA Application Stage 1 | Dec 2019
- What a Rural Generalist is
- How Rural Generalists support rural, remote and First Nations communities
- What Rural Generalist recognition means
- How to submit your response to the consultation.
Download the presentation slides here.

Practitioner Webinar
The National Rural Generalist Taskforce hosted a webinar on the recognition process for practitioners. Watch the recording via the link below using the passcode: NiSUV@u5

Community Webinar
The National Rural Generalist Taskforce and Rural Australians Matter hosted a webinar for the wider community on the recognition process and the opportunities to participate in the public consultation. Watch the recording via the link below using the passcode: qXU?K3R+
What is Rural Generalist Medicine?
Working as part of a multi-professional and multi-disciplinary team of colleagues, both local and distant, to provide services within a ‘system of care’ that is aligned and responsive to community needs.
(From the Cairns Consensus, International Statement on Rural Generalist Medicine, 2014).
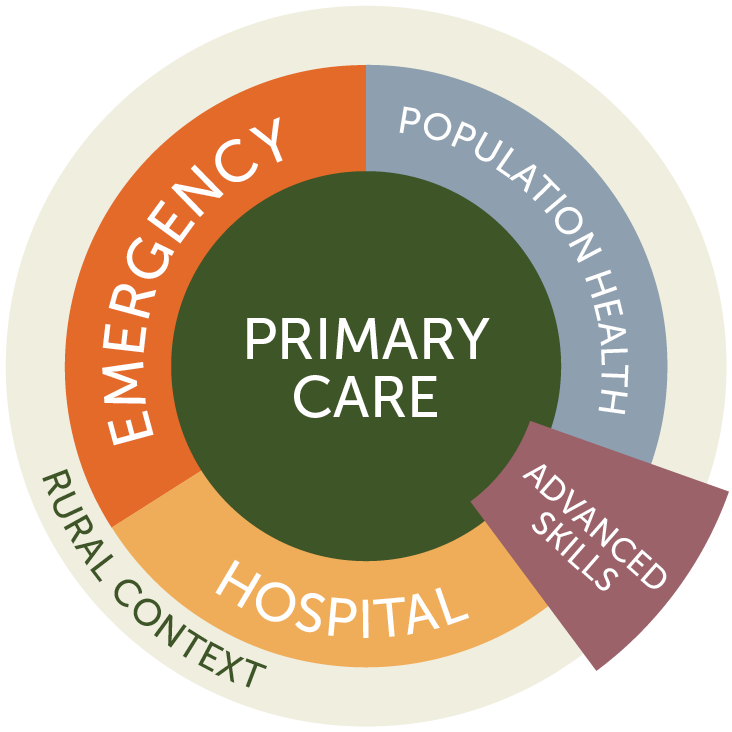
Rural Generalist Medicine is the provision of a broad scope of medical care by a doctor in the rural context that encompasses the following:
- Comprehensive primary care for individuals, families and communities
- Hospital in-patient care and/or related secondary medical care in the institutional, home or ambulatory setting
- Emergency care
- Extended and evolving service in one or more areas of focused cognitive and/or procedural practice as required to sustain needed health services locally among a network of colleagues
- A population health approach that is relevant to the community

What is a Rural Generalist Medical Practitioner?
A Rural Generalist medical practitioner is a General Practitioner who has specific expertise in providing medical care for rural and remote or isolated communities. A Rural Generalist medical practitioner understands and responds to the diverse needs of rural communities: this includes applying a population approach, providing safe primary, secondary and emergency care, culturally engaged Aboriginal and Torres Strait Islander peoples’ health care as required, and providing specialised medical care in at least one additional discipline.
Learn more about the College’s Rural Generalist Medicine Position Statement.
This video provides information on the National Rural Generalist Pathway, a training program to provide general practitioners with skills to meet the diverse health needs of regional, rural and remote communities. Hear from the former National Rural Health Commissioner, Adjunct Professor Ruth Stewart, and trainee rural generalist, Dr Preston Cardelli, about their experience in the rural generalist field and what attracted them to the role.
National Rural Generalist Pathway
In 2014 the Government announced its commitment to implementing a National Rural Generalist Pathway and appointed the National Rural Health Commissioner to progress this.
In 2019 a commitment of $62m was made toward the Pathway to support dedicated Rural Generalist training, including at the junior doctor stages and an application for professional recognition of Rural Generalism.
ACRRM began in 1997 in the hope that rural doctors could secure a national system to preserve their (Rural Generalist) model of practice and the College has fought ever since to achieve this. After 23 years, ACRRM is elated to see its programs are to be supported by a dedicated, national framework and continues to lead work to implement the pathway in a cooperation with key stakeholders.
The plan will operationalise the National Rural Generalist Taskforce Report recommendations presented by the National Rural Health Commissioner, Prof Paul Worley.
ACRRM co-led the Taskforce and its recommendations are closely aligned with ACRRM’s curriculum, standards and Position Statement and vision for the NRGP implementation.
The implementation of the NRGP is now overseen by the NRGP Strategic Council, which is chaired by the National Rural Health Commissioner, Professor Jenny May and includes representation from key peak bodies including ACRRM and commonwealth, state and Territory health services.

RG Reports & Research
- Murtupuni Statement on rural generalist practice in Australia (Nov 2024)
- RGR Overview - Presentation to NRGP (Aug 2023)
- Selecting RG Workforce (Jun 2023)
- OTTAWA Selection outcomes that count (Aug 2022)
- Case for MBS recognition of RG (Jul 2022)
- ACRRM Fellowship Articulating the Rural Generalist Medicine Standard (Sep 2021)
- National Rural Generalist Taskforce Report (Dec 2018)
- Rural Generalist Pathway Jurisdictional Mapping (Jul 2017)
- World Summits on RG Medicine (Apr 2017)
- The Rural Way (May 2014)
- International Statement for Rural Medical Generalism: Cairns Consensus Statement (Apr 2014)
- Rural Generalists Research Paper: This is a systematic review of the expanding role of generalists in rural and remote health. The paper was a research collaboration between ACRRM and the Australian Primary Health Care Research Institute of the Australian National University. (Nov 2007)

FAQs
A Rural Generalist is a medical practitioner who is trained to meet the specific current and future healthcare needs of Australian rural and remote communities, in a sustainable and cost-effective way, by providing both comprehensive General Practice and emergency care and required components of other medical specialty care in hospital and community settings as part of a rural healthcare team.
Rural Generalist Medicine is a specific approach to General Practice that is particularly relevant to rural and remote communities. The Rural Generalist Medicine body of skills incorporates the skillset of General Practice and is specifically shaped to optimise medical service capacity in rural and remote clinical contexts.
As rural and remote settings are characterised by their restricted access to the range of services, staff and resources available in urban centres, Rural Generalists are skilled to perform a broad range of medical services, including some skills, ordinarily within the province of other specialties. They are trained to apply these services effectively in a low resource environment, including working in local healthcare teams and providing local medical leadership in managing patient support from health care specialists in urban centres.
Rural Generalist practitioners are thus a key component of the multi-professional teams that together can deliver the highest quality care in rural and remote communities, Rural Health Multidisciplinary Teams are described in the Ngayubah Gadan Consensus Statement which may include other rural GPs, other medical specialists, nurses, Indigenous health workers and allied health practitioners.
- enable health services’ quality and safety and employment systems to consistently recognise and understand these doctors’ capacity and appropriately utilize their skills
- enable rural patients to better understand the training and capacity of their doctors
- simplify the processes for training, employment, and hospital credentialing for Rural Generalists (which are currently complex and onerous due to lack of coordination)
- provide a mechanism for Rural Generalists to be counted in rural workforce and resource planning
- focus academic effort to building the evidence-base for best practice Rural Generalist care
- make it easier to promote rural careers as RGs to the next generation.
An initial application for national recognition of Rural Generalist Medicine as a specialist field within the specialty of General Practice must is submitted to the Medical Board of Australia (MBA).
Stage 1 Initial assessment of application: The Stage 1 application describes the objectives of the proposal in broad terms. The MBA delegates to the Australian Medical Council (AMC) for assessment and advice and, following from this advice, determines whether a sufficient case has been made to demonstrate that the proposal is eligible to proceed to a Stage 2 assessment.
Stage 2 detailed assessment of application: A second application is submitted providing a more comprehensive overview of the proposal. The AMC assesses the detailed case for recognition of a new field of specialty practice on behalf of the MBA. This stage involves rigorous assessment of the case that includes a public consultation process and results in a recommendation being made to the Australian Health Ministers Committee for final approval.
The new or amended specialist field becomes an approved specialist field under the National Law and will be added to the approved List of specialties, fields of specialty practice and related specialist titles. The Medical Board of Australia (MBA) will then decide on the approved qualification/s in the new or amended specialty for the purposes of specialist registration. Medical Colleges with programs of study in that field can apply to have these programs accredited with the Australian Medical Council (AMC) as a qualification in the specialist field.
The programs will be assessed against the approved accreditation standards for specialist medical training programs. If the AMC accredits a program of study in the new or amended specialist field, it provides a report to the MBA that will determine whether to approve the program as providing a qualification in the new or amended specialist field for the purposes of specialist registration.
If the new or amended specialist field is recognised under the National Law, medical practitioners awarded an approved qualification in the recognised specialist field can apply for specialist registration. If a medical practitioner is granted specialist registration in the new or amended specialist field, it will be recorded in the Register of Medical Practitioners and the practitioner can use the protected title associated with the specialty.
As Rural Generalist Medicine is a specialist field within General Practice. It is expected that doctors with a nationally accredited qualification in this field would be both registered as specialist General Practitioners and specialists in Rural Generalist Medicine.
The public can search their doctor’s specialist registration details on the national Register of Practitioners. The public register provides assurance that medical practitioners with specialist registration are qualified in the recognised specialty. It also confirms that they have professional indemnity insurance and are complying with continuing professional development and recency of practice requirements.
The general practice colleges have different models for delivering rural generalist training.
- The ACRRM Fellowship qualification (FACRRM) is AMC accredited as a general practice qualification and is designed to reflect attainment of the requisite professional standards for the practice of Rural Generalist Medicine.
- RACGP has introduced a FRACGP-RG Fellowship qualification which is a general practice qualification designed to reflect the standards for Rural Generalist Medicine.
The two general practice colleges, ACRRM and RACGP, currently provide the training, continuing Professional Development and Fellowship qualifications which the Medical Board of Australia recognises for Vocational Registration purposes for specialist general practitioners. As Rural Generalist Medicine if recognised would be a specialist field within general practice, these existing arrangements would be extended to also apply to the new field.
This is the name the Commonwealth Department of Health have given to their commitment to constructing a national framework to support doctors to train, qualify and practice as rural generalist practitioners in a way that is structured and consistent and which enables portability across health services and jurisdictions.
Ultimate determinations will rest with the national committee of health ministers with advice from the Medical Board of Australia (Board).
If Rural Generalist Medicine is recognised as a new specialist field within general practice under the National Law, then doctors awarded an approved qualification in Rural Generalist Medicine will be able to apply for specialist registration in that field.
ACRRM RG Fellowship Program will be assessed through the AMC processes, and it is expected that it will be accredited and FACRRM will become an approved qualification in the new specialist field of Rural Generalist Medicine. Currently, the ACRRM Fellowship Program is AMC accredited, and the FACRRM is an approved qualification, in general practice.
It is anticipated that as a FACRRM you would then be able to apply through Ahpra for registration as a specialist Rural Generalist and this would be held in addition to your registration as a specialist general practitioner. Specialist registration in the new field of Rural Generalist Medicine, would be recorded in the Register of Medical Practitioners and would entitle you to use the protected title associated with the specialty.

